CAN ARTIFICIAL INTELLIGENCE PREDICT THE RISK OF PANCREATIC CANCER USING DISEASE TRAJECTORIES?
Researchers used artificial intelligence (AI) approaches on real-world longitudinal clinical data to build monitoring programmes for the early diagnosis of individuals at high risk of pancreatic cancer, one of the most aggressive illnesses.
CONCERNING
THE RESEARCH
The current study employed real-world longitudinal health records from a large number of patients to identify several people at high risk of pancreatic cancer.
They used
patient information from the Danish National Patient Registry (DNPR) and,
later, the United States Veterans Affairs (US-VA) Corporate Data Warehouse
(CDW) to apply freshly discovered machine learning (ML) algorithms.
The former
included clinical data from 8.6 million patients between 1977 and 2018,
equivalent to 24,000 pancreatic cancer cases, and the latter included clinical
data from three million patients, corresponding to 3,900 pancreatic cancer
cases.
The researchers developed and evaluated a wide range of machine learning models on the sequence of illness codes in the DNPR and US-VA clinical data, as well as the prediction of cancer incidence.
>> click here>>https://39961kfnglu-5z1wsny7oyyk2p.hop.clickbank.net
BACKGROUND
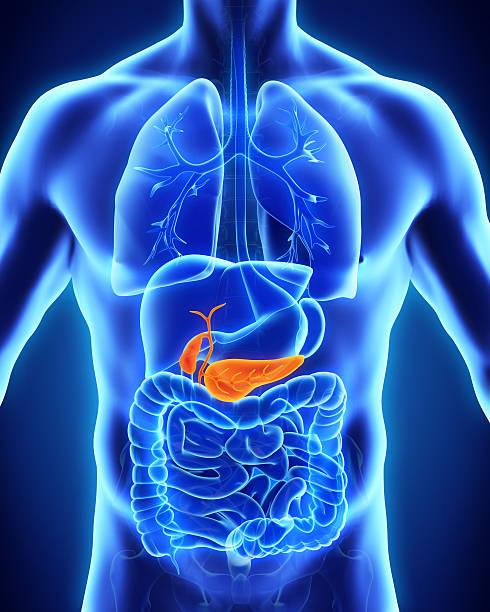
Pancreatic
cancer is becoming more common, making it the top cause of cancer-related
fatalities globally. Pancreatic cancer is difficult to detect due to a lack of
awareness of its risk factors.
Late identification at advanced or remote metastatic stages complicates therapy, making patient survival exceedingly rare. At five years, just two to nine per cent of such patients survive.
Although age
is a known risk factor for pancreatic cancer, age-based population-wide
screening is impracticable due to the high expense of clinical testing, which
also produces false-positive findings.
Furthermore,
data on family history or genetic risk factors for the general population are frequently
lacking. As a result, there is an urgent need to create low-cost monitoring
programmes for early diagnosis of pancreatic cancer. In developing prediction models, the researchers employed
three-character International Classification of Diseases (ICD) diagnostic codes
and classified 'pancreatic cancer patients as those who had at least one code
under C25, signifying malignant neoplasm of the pancreas.
Cancer
diagnostic illness codes were 98% accurate. Finally, the researchers identified
which diagnoses in a patient's history of diagnostic codes were most revealing
of cancer risk to recommend an optimal monitoring program.
CLICK HERE >>>https://fadc4mchm91550eag472i63yco.hop.clickbank.net
Furthermore, the researchers used the area under the receiver operating characteristic (AUROC) and relative risk (RR) curves to assess the prediction performance of the various models trained in the DNPR. Furthermore, they revealed ML-derived RR ratings of cancer patients in the high-risk category.
OUTPUT
All prior
research that used real-world clinical records to predict pancreatic cancer
risk yielded good findings, but they did not extract time-sequential
longitudinal characteristics from illness histories. They tested
non-time-sequential models on the DNPR dataset in this work.
While clinicians may have discovered some instances based on known pancreatic cancer risk factors, such as chronic pancreatitis, a significant portion of them, approximately 70, would still be newly diagnosed based on a conservative estimate.
>>Click here>>https://d5797flddit8498vtnqcs1opei.hop.clickbank.net
Despite the
use of common ICD illness codes and similar cancer survival, cross-applying the
DNPR data to the US-VA data reduced the performance of ML models, emphasizing
the requirement for independent model training across geographical areas to
achieve regionally optimal model performance.
However, an
ideal environment for multi-institutional collaboration to achieve globally
relevant results
CONCLUSIONS
The accuracy of the ML-based models reported in this paper might increase with the availability of data other than illness codes, such as observations documented in clinical notes, test findings, genetic profiles of additional people, or health-related information from their wearable devices.
Then, clinical
adoption of early pancreatic cancer detection would necessitate the
identification of high-risk individuals.
Because
individuals at the highest risk are a smaller subset of a huge population
computationally assessed, costly and improved clinical screening and
intervention programs will be restricted to a few people.
Nonetheless,
AI on real-world clinical records has the potential to change the focus from
late-stage cancer treatment to early-stage cancer treatment, which would
significantly enhance the quality of life for all patients while raising the
benefit-to-cost ratio. Finally, utilizing disease
trajectories, artificial intelligence (AI) has the potential to be a helpful
tool in forecasting the risk of pancreatic cancer. Large volumes of data, such
as a patient's medical history and imaging findings, may be analyzed by AI
algorithms to detect trends and make predictions about a patient's future
health outcomes.
click here>>>> https://0c7d6omklk0yx09fsrje0k7ucq.hop.clickbank.net
Healthcare practitioners may be able to identify individuals who are at a higher risk of getting pancreatic cancer early by utilizing AI to analyze disease trajectories, allowing for earlier intervention and maybe improved treatment results. Furthermore, AI may be able to assist in the personalization of treatment strategies for specific patients based on their distinct disease trajectories.
While more
study is needed in this area, the prospective benefits of employing AI in
pancreatic cancer are promising. Risk
prediction appears to be promising. As AI technology advances and more data
becomes accessible, AI is anticipated to play a growing role in improving
patient outcomes in the battle against pancreatic cancer.
PLEASE COMENT;>>>>>>>>>>








Comments
Post a Comment